Shot or Not? Everything You Need to Know About the COVID-19 Vaccine in January
January 23, 2021
As the COVID-19 pandemic rages into its twelfth month, much of the discourse has been turned to the future, a future without COVID-19.
A month ago, The Tritonian covered the initial development and release of Pfizer’s COVID-19 vaccine.
In the time since, several other companies, including Moderna, AstraZeneca, and now Johnson and Johnson, have also released American-approved vaccines, setting the stage for a hopefully quick, decisive end to the pandemic.
Now that vaccines exist, the conversation has largely turned to distribution.
The United States Center for Disease Control has released recommendations for how states should distribute their vaccines.
In response, Wisconsin has broken down its vaccine distribution plan into three population categories of high risk groups, in descending order of priority.
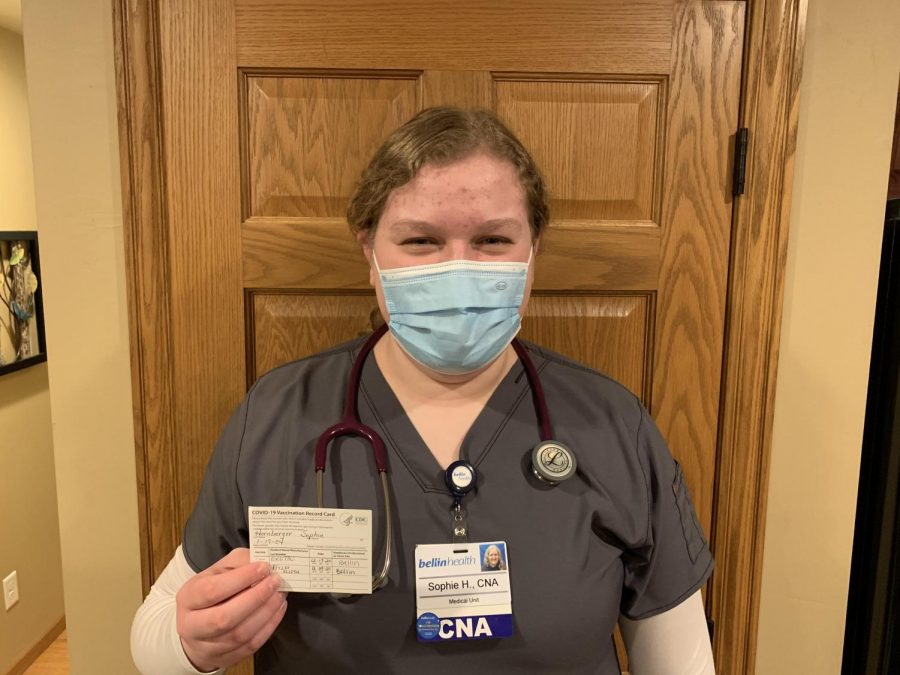
Phase 1a includes frontline healthcare workers, first responders, and long term care residents/staff.
Phase 1b, if approved in its current form, will include all Wisconsinites aged 65 or older, along with other important demographics, such as educators, food chain workers (grocery workers, agricultural workers, food pantry staff, etc.), corrections workers, public transit workers, social workers, 911 dispatchers, frail elders and adults with disabilities in Wisconsin’s IRIS and Family Care programs, and mink farmers.
As of January 22, the Wisconsin Department of Health Services has confirmed the state is on track to receive 70,000 doses weekly.
Earlier this week, the vaccine was first made available to people ages 65 and over, a population of approximately 700,000 Wisconsinites, putting the state on pace to fully vaccinate this demographic in ten weeks.
The move to Phase 1b, as described above, would require the vaccination of an additional 560,000 people.
If production levels remain the same and the plan is approved in its current form, this would likely be achieved seventeen weeks from now.
However, if vaccine production and distribution improves, these timetables may shrink.
“We are fortunate because our local health partners are ready to vaccinate as many people as they can as soon as they receive the medication,” said NDA School Nurse Amy Rader BSN, RN.
“We are expecting Phase 1b to be approved and go into effect any minute, but vaccine supply has become a big issue. At this time, it is hoped that NDA faculty and staff would be able to get vaccinated by the start of next school year. We are certainly hoping it will be sooner, but there are no guarantees. Health systems are only allotted so many vaccines by the federal and state government per week of the 70,000 total. There are over one million people in the grouping of 65+ years olds and people in Phase 1b, so it will take time to get two shots in each person who chooses to vaccinate,” she explained.
Much of the future now relies on how quickly vaccines can be produced, and subsequently distributed.
To this effect, in a flurry of executive actions yesterday, President Biden invoked the Defense Production Act, a Korean War-era law that allows the federal government, like in war time, to mandate select private manufacturers to halt production of “unneeded” goods, and instead, ramp up production of the COVID-19 vaccine.
The hope among the medical community is that such actions will allow vaccines to be produced on a much larger scale, allowing the country, and the world, to achieve herd immunity at a faster rate than currently projected.
“The ultimate goal of vaccination is to help protect us while living through the pandemic. We hope to prevent the spread of the virus, which in turn helps prevent sickness and death. Even if you are vaccinated, there is a chance you could carry the virus, and that is why it is recommended so many people get the vaccine. The more people who vaccinate, the fewer people are left to be susceptible to contracting the illness, encouraging what’s known as ‘herd immunity,’” said Rader.
The COVID-19 vaccine, though, certainly hasn’t come without its own share of controversy.
“If an individual is concerned or wants more information, we are encouraging them to ask their own healthcare providers. We know this is a new disease and a new vaccine, and it is hard to know which information is credible. But, there is a lot of solid research and credible information out there. Trusting Facebook or other social media outlets, though, is not likely to provide the best or evidenced-based information. The best choice is talking to people who understand the science behind the vaccine when making a decision whether or not to get yours,” she continued.
Wisconsin’s Catholic Bishops have also taken to the stand in support of vaccination, explaining “Catholics have a responsibility to promote the common good in society, act in solidarity with our neighbor, and protect human life…vaccination is one means of demonstrating love of our neighbor.”
This article was made possible through the medical expertise of the following:
Amy Rader BSN, RN, NDA School Nurse
Michael LaMere, MS, LAT, NASM-PES, Prevea Health Manager
Mark Husen, LAT, Bellin Health Team Facilitator